Uterine sarcomas are a class of relatively rare but particularly deadly uterine cancers, which have recently emerged at the heart of a major healthcare controversy over surgical devices called power morcellators.
These once-popular devices have fallen out of favor after the FDA warned the public that they can cause undiagnosed uterine sarcoma to spread through a patient’s body, significantly worsening prognosis.
Characteristics of Uterine Sarcoma
Cancers are generally classified by their area of origin and uterine sarcoma arises from either the smooth muscle or connective tissue of the uterus.
That is, it develops in the myometrium rather than in the endometrium (the mucous membrane lining) of the uterus, features shown in the diagram below.
Uterine sar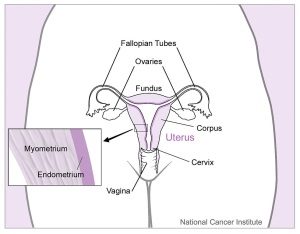 comas comprise only about 3% of all uterine cancers. Cancers of the endometrium, called carcinomas, form the majority of uterine cancer cases.
comas comprise only about 3% of all uterine cancers. Cancers of the endometrium, called carcinomas, form the majority of uterine cancer cases.
However, uterine sarcomas are also much harder to diagnose and treat, and are associated with a poorer prognosis in comparison to the more common carcinomas, for several key reasons.
1. Rarity Means Doctors Have Less Experience with Sarcomas
Because there are relatively few cases of uterine sarcoma, most doctors have little or no direct experience to help them diagnose and treat the disease. Many doctors send biopsies out to experienced histologists when faced with a suspected sarcoma.
The fact that fewer case studies of sarcomas exist also makes it more difficult to gauge the efficacy of treatment methods.
2. Common Screening Methods Inapplicable or Ineffective
- Radiological Imaging Methods. Sarcoma tumors can be seen in MRI or CA
 T scans. However, they can look nearly identical to uterine fibroids, which are exceedingly common benign uterine growths Doctors highly experienced with uterine sarcoma tumors can usually differentiate them from fibroids, but some sarcomas simply appear too similar for reliable identification. Also, radiological scanning is relatively expensive and it would be prohibitive for most hospitals to run them on every prospective uterine surgery patient.
T scans. However, they can look nearly identical to uterine fibroids, which are exceedingly common benign uterine growths Doctors highly experienced with uterine sarcoma tumors can usually differentiate them from fibroids, but some sarcomas simply appear too similar for reliable identification. Also, radiological scanning is relatively expensive and it would be prohibitive for most hospitals to run them on every prospective uterine surgery patient. - Risk Factor Analysis. Many risk factors for uterine fibroids overlap with those for uterine sarcoma. This is part of why some critics of power morcellator feel that it’s too risky to ever use a power morcellator for fibroid treatment surgery, especially when alternative surgical options or non-surgical treatment methods are available.
- Pathological Testing of In-Office Biopsy or Swab. Since sarcomas attack the smooth muscle, it’s not possible use an in-office swab for testing, as the cancer will only be detected in the sample if the disease has already spread to the uterine lining.
- Pathological Testing of Surgical Biopsy. This is the only reliable method of diagnosing a uterine sarcoma. Yet it is not feasible to use surgical biopsies as a routine screening method for uterine sarcomas. One problem in such an approach is that undergoing surgery for testing prior to a fibroid treatment surgery would expose the patient to more inherent mortality risk from surgery. Also, selecting which areas to biopsy is challenging because cancerous tissue can be hidden deep within.
3. Sarcomas are Aggressive
Uterine sarcomas are known to be aggressive cancers, which indicates three main characteristics:
- Quick Spread of Cancerous Tissue from the Site of Origin. A rapid rate of spread means that the cancer progresses faster than less aggressive cancers and is more difficult to treat, especially with localized treatments such as surgical excision.
- A Tendency for Recurrence. While surgical excision is currently the recommended treatment method for sarcomas, it generally requires the surgeon to remove a large margin around the tumor site to be completely successful. Yet it can be hard to tell exactly how far around the tumor the cancer has spread. Unfortunately, If some cancerous tissue remains in the tumor site, or lies hidden in another area, the cancer can quickly recur.
- Poor Prognosis. Because of the previously-mentioned characteristics, and also because uterine sarcomas tend to be resistant to common treatment methods such as chemotherapy and hormone therapy, life expectancy and quality of life for sarcoma patients are often predicted to be very limited, even with a comprehensive treatment plan.
How Do Morcellators Aggravate Uterine Sarcoma?
It is important to note that power morcellators do not cause uterine cancer. The patients affected by morcellators already had uterine sarcoma before their surgeries, though they were unaware of it.
But if, as these patients claim, they showed no outward symptoms of cancer prior to surgery, it’s likely that their undiagnosed cancer was at an early stage at the time, meaning that malignant tissue was probably concentrated in only one or a few places in the body.
Herein lies the potential threat that power morcellators pose to patients: the spinning blades of the devices can fling bits of cancerous tissue all over the patient’s organs and other internal structures. This can cause cancer to take root in new locations, accelerating the progression of the disease to an advanced stage.
Tragically, numerous patients have died from cancer within a year of receiving power morcellation. Without morcellation, they may have had a much higher chance of fighting their disease, as early stage cancers respond better to treatment.
Have You Been Harmed by a Power Morcellator?
If you or someone close you received a uterine cancer diagnosis after undergoing a hysterectomy or myomectomy involving a power morcellator, you may be entitled to significant compensation for your pain and suffering.
More than 20 lawsuits have been filed throughout the country by victims of power morcellation against device manufacturers, doctors, and hospitals who allegedly misinformed or failed to warn patients of the risks.
Every power morcellator case is highly individual, so it is best to consult with legal counsel to determine the viability of your case. Contact Monheit Law today for a case evaluation with our experienced lawyers, at no cost.
